February 2019 Independent Eating and Drinking Newsletter
| Independent Eating and Drinking are Wonderful |
 |
| February Newsletter Topics: |
|
| Subscribe to Newsletters |
The Benefits of Independent Eating
Independent eating is something that most cultures consider an important activity of daily living. It is not always fully understood that people who are unable to feed themselves can benefit greatly if they can gain control over eating. The activity of eating influences many of the known psychological benefits associated with greater independence, such as improved dignity and self-esteem, and reduced feelings of being a burden to their caregiver (Gustafsson)1. Hermann, et al.2, supports a similar view stating that “eating activity influences many aspects of our overall medical, physical, and social well being”. The ability of food self-selection and the capacity to set ones own pace in eating can potentially ameliorate some of the undernourishment and/or gastric problems, as well as some of the risks of being fed, that often occur for people who are fed.
We all start out our lives being fed. During the first year or two of life most people develop the skills necessary to feed themselves. Eating becomes an automatic activity that is given little or no conscious thought. However, some people are unable to develop the skills needed to self-feed due to a variety of causes and being fed is continued out of necessity. This group will potentially be dependent upon another person for all of their nutritional needs, and in some cases, for hydration, for their entire life.
An additional group of people, who have been independent eaters, lose the ability to self-feed due to illness or injury and become dependent upon another person to feed them and, often, to also provide them with fluids. To facilitate mealtime independence it must be understood that for those who have never experienced independence in eating, the perception of self-feeding is different from those people who have had self-feeding experience. Therefore, teaching someone, who lacks familiarity with self-feeding, to feed them self must be approached with that understanding. If food has always been placed in their mouth without them being required to participate in removing the food from the utensil, they will not understand the concept and will have to learn it before they will be able to gain any degree of independence.
Potentially, many individuals from both groups of people can gain the ability to eat and drink independently through the use of assistive technology (AT). However, it is common to find that many caregivers including family members (especially older members), paid caregivers, and healthcare insurance company reviewers do not see a need for, and are resistant to, making this change. Yet, eating independently can be justified as being medically necessary for many physical and psychological reasons. (Medical necessity will be discussed in detail in a future Newsletter. If you need assistance with this subject, please contact us.)
AT can range from a simple non-slip mat placed under a plate, to a custom built splint, all the way to sophisticated powered dining equipment like the Mealtime Partner Dining Device. Unfortunately, there is a common misconception that empowering someone with mealtime independence is simply a convenience to the caregiver and provides no significant benefit to the consumer and, therefore, is unessential. Because this is such a predominant misconception, the benefits of independent eating will be discussed in detail starting with safety and health issues.
Safety Issues. The greatest safety benefit of eating and drinking independently is that it reduces the chance of choking and/or aspiration. There are approximately 40,000 deaths in the U.S. each year due to aspiration pneumonia with a cumulative cost of treatment that is estimated to be more than $3 billion (Calhoun, Wax & Eibling3, DeLegge4). DeLegge’s study identified the best predictors for the development of aspiration pneumonia as: dependency on others for eating; dependency for oral care; neurological status; and position while eating. Fundamentally, people who require feeding are more vulnerable to aspiration than people who self-feed. (Aspiration occurs when food, liquid or regurgitated gastric materials are inhaled into the pulmonary system. Pneumonia can result from aspirated materials causing infection in the lungs and can have very serious health consequences.)
Proper positioning for the task of eating can reduce this risk. Simply controlling when food and/or liquid is placed in the mouth, enables a person to be more prepared to receive the food or liquid. Their sequence for breathing will better coordinate with the placement of food in their mouth, and, consequentially, reduce the risk of aspiration.
When one is being fed it is not always easy to know exactly when food is going to be placed in your mouth. Those providing food can change their mind and pause, or alternatively, speed up the food presentation depending upon what is occurring at the time. Also, they might change the angle at which the utensil is presented. Furthermore, if the person providing the food is in a hurry they might feel compelled to rush the meal. This is an especially common occurrence in facilities like nursing homes. Presenting food hurriedly, typically results in the person being fed taking the food from the utensil, regardless of whether or not they are ready for it. They will continually take the food when it is offered, even if they have not swallowed the previous bite. This pattern increases the likelihood of choking and/or aspiration.
Health Issues. Hurrying food consumption impacts most people’s digestive system and results in heartburn, indigestion or acid stomach (most of us have, at one time or another, experienced having a hurried meal and then feeling the need for an antacid). Gastro esophageal reflux disease or GERD, commonly referred to as acid reflux, is a condition in which stomach liquids regurgitate into the esophagus and, over time cause damage to it. Many people, who are constantly hurried during eating, develop GERD.
It is common for older people to require a protracted time to eat even a small meal. However, in many institutional settings they are required to eat quickly (generally due to staff shortages at mealtimes), and the result is indigestion following a meal, and over time, the development of GERD. The long term consequence is that the person is reluctant to eat because their stomach is upset and they are in pain. This can cause a downward health spiral with weight loss and under nutrition as the result.
Under nutrition and malnutrition exist at epidemic proportions in nursing homes in the U.S. The American Geriatric Society and the Nutrition Screening Initiative identified that approximately 40% of all nursing home residents are under nourished. A report titled Malnutrition and Dehydration in Nursing Homes: Key Issues in Prevention and Treatment5 established the key reasons as being: residents must be fed, or need help eating; the need for additional time to eat; cognitive impairments; and, chronic understaffing in nursing homes.
Conclusion: The benefits of independent eating are considerable and diverse. This article has only touched on a few points. If you have questions or comments please let us know. Call us at 800-946-8607, or email info@mealtimepartners.com.
|
Whether it is eating or drinking Mealtime Partners has a HANDS-FREE solution to independence |
|
 |
 |
| The Mealtime Partner Dining System on Legs | The Front Mounted Drinking System |
Independent eating, whether it is accomplished in the traditional way, using your hands, or using assistive technology, allows you to select the order in which the various foods that are being served are eaten, and also the pace at which each bite is eaten. Thus, meats can be chewed for however long it takes to break the bite into particles that are easy to swallow, while the soft food, like pudding, can be swallowed quite rapidly. The Mealtime Partner Dining System allows those individuals who cannot feed themselves using their hands and a utensil, to be able to control their mealtime completely. They can change the pace of eating to accommodate the textures of food that are being eaten, and also to pause to interact with other diners. Additionally, plenty of water should be consumed, all day long. For those individuals who are unable to pick up a cup, maintaining healthful consumption of liquids can be difficult. Mealtime Partners products provide a solution. For more information about our drinking products, please visit the Drinking page on the Mealtime Partners website. |
|
| For more information about the most flexible assistive dining system available, please visit: The Mealtime Partner Dining Device Description webpage, or call us at 800-996-8607. | |
The Hydration Backpack with Drinking Tube Positioning
Because hydration is so important to good health, Mealtime Partners is emphasizing the use of hands-free drinking systems to facilitate consuming enough liquids for those who are unable to independently take a drink. In last months Newsletter the Drink-Partner Drinking System was discussed. To continue providing details about our unique line of drinking products, this month we will describe the Hydration Backpack with Drinking Tube Positioning. In next months Newsletter, information will be provided about the Hydration Backpack with Drink Tube Positioning that can be used on powered wheelchairs that have slide-tracks for mounting accessories. Figure 1 shows the Hydration Backpack with Drinking Tube Positioning mounted on a manual wheelchair.
 |
| Figure 1: The Hydration Backpack with Drinking Tube Positioning Attached to a Manual Wheelchair |
The components of the Hydration Backpack with Drinking Tube Positioning are pictured in Figure 2. The backpack is an insulated canvas bag with shoulder straps and a carrying handle at the top. The canvas bag contains a 70-ounce bladder. A drinking tube extends from the base of the bladder and passes through a slot in the shoulder strap of the backpack. At the end of the drinking tube is the bite valve assembly which contains an on/off valve (i.e., switch, operated by hand) and a bite valve operated by the user by biting on it. When bitten, the opening in the bite valve opens to release liquid (assuming the on/off valve is turned on).
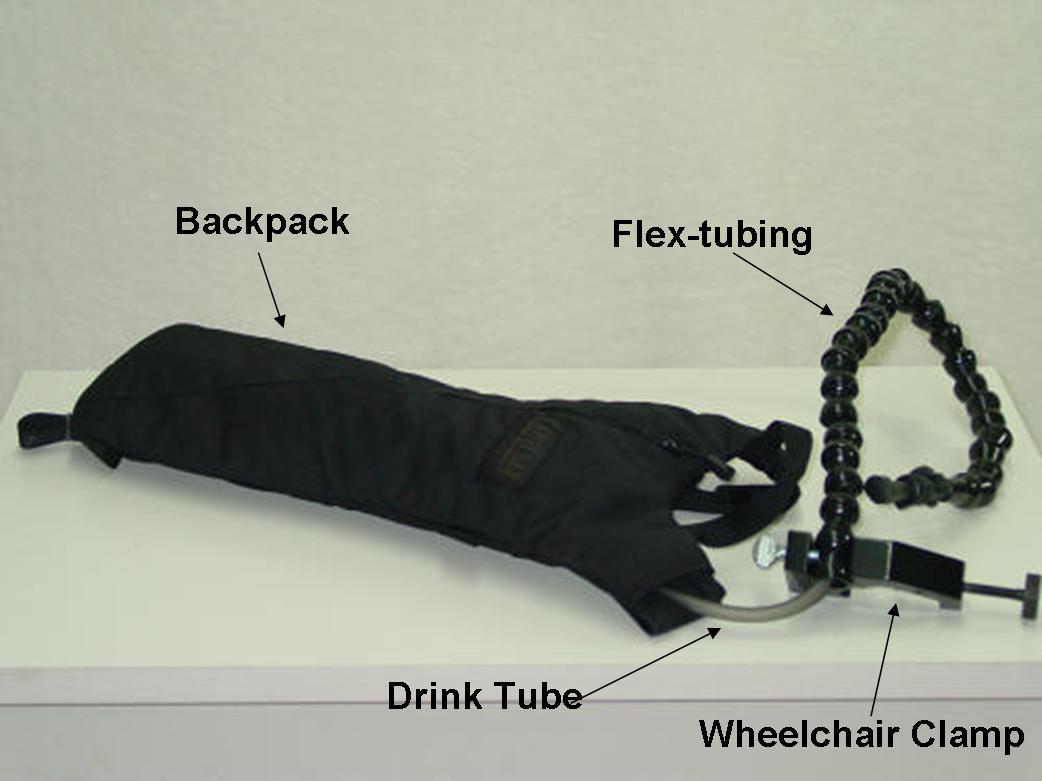 |
| Figure 2: Components of the Hydration Backpack with Drink Tube Positioning |
The backpack can be mounted on the back of a wheelchair. If the wheelchair has handles, the shoulder straps are looped over the handles and the backpack rests behind the seat and is relatively flat and unobtrusive (as shown in Figure 1). If the wheelchair does not have handles (like some powered wheelchairs), the backpack can be attached to the wheelchair using the handle on the top of the bag and looping it over the Wheelchair Clamp once it is attached to the wheelchair frame.
Once the backpack is in position, the Wheelchair clamp should be attached to one of the wheelchair handles. The Wheelchair Clamp has two clamping areas, a large clamping area for attaching to the Wheelchair structure and a smaller clamp to hold the Flex-tubing. Position the wider opening of the clamp around the Wheelchair handle with the screw knob positioned vertically so it won’t interfere with anything or prohibit mobility. Tighten the screw until the clamp is firmly attached to the handle as shown in Figures 3. (Needless to say, the clamp can be located on either side of the wheelchair to suit the preferences of the user.) The clamp should be positioned with the second, smaller clamp opening, above the handle. Loosen the thumb-screw on the top of the clamp until none of the threads are visible inside the clamp opening when installing on the wheelchair. Slide the Flex-tubing into the clamp opening from the front of the wheelchair to the back. After one link of the tubing is in the clamp, align the indent in the Flex-tubing with the thumb-screw and tighten it until the tubing is held firmly in place.
 |
| Figure 3: Wheelchair Clamp Attached to Handle of a Wheelchair |
Flex tubing is easily formed into almost any number of straight or curved shapes. Form the Flex-tubing to come forward over the user’s shoulder, loop down towards their chest and then bend back upward, positioning the bite valve slightly below the user’s mouth as shown in Figure 4. Depending upon how much head, neck and trunk movement that the user has, the bite valve can be put very close to the user’s mouth or positioned to the side, or farther away.
 |
| Figure 4 - Flex-tube Positioned for User Access |
This drinking system is flexible enough that it can also be mounted to either a wheelchair with no handles, or to a bed. To mount the system on a wheelchair with no handle, attach the Wheelchair Clamp to a structural tube on the chair that is preferably at the user’s shoulder level. After the clamp is attached, slip the handle at the top of the backpack over the clamp making sure that it is securely positioned. When the backpack and clamp are in place, insert the Flex-tubing into the clamp as described earlier, and position the bite valve appropriately for the user. Similarly, the drinking system can be attached to the rail of a bed or a bed headboard. Thus, liquids are available to a user all of the time.
It should be noted that once the Flex-tubing is formed into position it will hold its position until it is adjusted. However, should the user move forward and strike the tube, it will not resist the force and will move with the user. The tubing has no sharp edges and moves fluidly, and this provides a safety mechanism for all users.
It is recommended that this system be used to provide water to the user, rather than juices, cola’s, or sports drinks. This is because it is a more complex system to clean than a cup or mug that would be used in the Mealtime Partners Front Mounted Drinking System. The bladder, tubing and bite-valve need very thorough cleaning to prevent the growth of bacteria in the bladder and drinking tube. It will require more frequent cleaning if anything other than water is put into the drinking system. Detailed instructions for cleaning the Hydration Backpack with Drinking Tube Positioning are provided with each drinking system.
Follow this link to purchase a Hydration Backpack with Drinking Tube Positioning. If you have additional questions about the Hydration Backpack with Drinking Tube Positioning, please email Mealtime Partners at questions about drinking systems, or call us at 800-996-8607. We will be happy to discuss whether this drinking system will be able to meet the needs of a specific user.
|
Did you know? Did you know that scientists from the Sorbonne University in France have found that there is a correlation between consuming high quantities of ultra-processed food and an increased risk of death? Foods that are described as ultra-processed include a wide range of ready prepared foods that contain chemical additives that are not typically used in cooking. The chemicals are used to mimic the flavors of the real food products. Ultra-processed foods include a wide range of snacks (e.g., chips, cookies, baked goods, etc.), “heat and eat” meals, soft drinks, fish and chicken nuggets, and many more products. In a study of 44,551 individuals over 45 years of age, it was found that a 10% increase in the consumption of ultra-processed foods related to a 14% increase in mortality from all causes. Further research will be needed to identify the specific items in ultra-processed foods that are responsible for the increase in mortality, yet the current information does inform us that we should avoid eating very much ultra-processed food. |
February 2019 Newsletter References
1. Gustafsson B. The Experiential Meaning of Eating, Handicap, Adaptedness, and Confirmation in Living With Esophageal Dysphagia. Dysphagia, Spring, 1995, 10(2):68-85.
2. Hermann, R. P., Phalangas, A. C., Mahoney, R. M. Powered feeding devices: an evaluation of three models. Arch Phys Med Rehabil, 1999, 80: 1237-1242.
3. Calhoun, K. H., Wax, M., Eibling, D. E., Expert Guide to Otolaryngology. American College of Physicians, American Society of Internal Medicine. Publishe ACP Press, 2001.
4. DeLegge, M. H., Aspiration pneumonia: Incidence, mortality, and at-risk populations. Journal of Parenteral and Enteral Nutrition, Nov/Dec, 2002.
5. Greene Burger, S., Kayser-Jones, J., Prince Bell, J., Malnutrition and Dehydration in Nursing Homes: Key Issues in Prevention and Treatment. Published by: National Citizens’ Coalition for Nursing Home Reform, June 2000.
6. A videofluoroscopic swallow study (VFSS) is a procedure performed using medical imaging technology. During the test, the patient sits next to x-ray equipment and is fed a variety of foods and liquid mixed with barium. The barium makes the food or drink visible during x-ray. The x-ray equipment records a video of the movement of the barium.